|
|
The Riverbend Down Syndrome Association is a now a 501(c)(3) non-profit organization and can receive tax deductible contributions. Our Employer Identification Number is: 14-1982424.
We thank Dr. David R. Musich, DDS, Musich & Associates in Schaumburg, IL for this orthodontics newsletter issue.
We encourage all to attend the DSAGSL Buddy Walk. This event is the major fundraiser of the year of the Down Syndrome Association of Greater St. Louis.
The 2nd Annual Scotch Doubles Down Syndrome Bowling Tournament will be on Saturday, October 20, 2007 at the Tri County Bowling in Jerseyville. Two sessions at 2:00 and 5:00 p.m. $20.00 per couple if registered by October 10; $25.00 after the 10 th. Door Prizes will be awarded and 50/50 and raffles. Prizes: 1 st - $100, 2 nd - $75, 3 rd - $50. We have a very big goal to beat from last year so any support we get would be greatly appreciated. We need the following:
- Lane Sponsors - $100.00 (This gets the companies name at the end of one of the lanes.)
- Donated items to be raffled off.
- Donated items to be handed out as door prizes at both sessions.
- Help working the tournament that day.
If you have any questions or would like to help please contact Eric & Joy Stemmler, E-mail: stemmler3@frontiernet.net.
Local Events
September 1, 8:30 a.m. - 12:00 p.m. DSAGSL Buddy Walk. Free event in Forest Park, Muny Opera upper parking lot, followed by a party with bounce houses, entertainment, food and drink, awards and sponsorship booths. T-shirts will be available for sale for $10 each.
September 2, 10:30 a.m. - 1:15 p.m. DSAGSL Walk in the Park. Busch Memorial Stadium pregame rally, walk around the stadium warning track, and Cardinals game to celebrate this lives and accomplishments of people with Down syndrome in our area; broaden awareness throughout our community; and to foster positive attitudes of all people with Down syndrome.
|
 |
September 28, 11:00 a.m. Puttin' for DS. The third annual charity golf scramble will be held at Clinton Hill Golf Course in Swansea, IL.
Dinner and silent auction will follow. Lunch, cart, drinks, and prizes will be included. Proceeds to benefit St. Louis Children's Hospital Down Syndrome Center and the Down Syndrome Association of Greater St. Louis. For more details, contact Tim Nienhaus E-mail: puttinfordownsyndrome@yahoo.com or (618) 799-8515.
Down Syndrome Articles
Intervention and Patients with Down Syndrome. The Role of Inclusion, Technology and Leadership. Guest Editorial by David R. Musich. Current President of The Edward H. Angle Society of Orthodontists, Inc. The Angle Orthodontist: Vol. 76, No. 4, 2006, pp. 734-735. © Copyright by E. H. Angle Education and Research Foundation, Inc. 2006. Reprint permission granted by Robert J. Isaacson, DDS, MSD, PhD, Editor, Angle Orthod.
According to the Centers for Disease Control and Prevention (January 6, 2006 report) the prevalence of children born with Down syndrome (DS) in the United States is approximately 1:733. At this rate of occurrence, the genetic trait of trisomy 21 (DS) has a prevalence very similar to that of cleft lip and palate. Whereas dentistry and orthodontics have long been committed to the interdisciplinary team management of patients with cleft lip and palate, the dental/orthodontic commitment to patients with DS is less evident. A quick review of the two major orthodontic journals (American Journal of Orthodontics and Dentofacial Orthopedics and The Angle Orthodontist) illustrates the point—there have only been three articles published related to treatment of patients with DS in the last 25 years. In contrast, for cleft lip and palate treatment and research, during the same time period and for the same key orthodontic journals, approximately 50 articles were published.
|
|
|
Before and particularly since the passage of the Americans With Disabilities Act of 1976, parents of patients with disabilities have sought more inclusion for their children in both the educational setting and the medical setting. One generation ago, a large percentage of children born with DS died early in life because of cardiac problems, and many of those who survived their early medical problems were institutionalized as young children. Most of the current generation of parents of children with DS make a significant effort to include their DS children in many aspects of traditional family life, school, and sports. In addition, better educational mechanisms exist to assist them and their children medically and socially. Medical support groups and parent support groups have been very active in optimizing the quality of life for children with DS. The combination of these changes over the past few decades has led to a 100% increase in the life expectancy of persons with DS (from a previous average life expectancy of 30-40 years to a current life expectancy of 60-70 years).
There are many dental conditions common to children with DS that are well suited for orthodontic intervention and should be considered for correction at the appropriate times.1,2
- Maxillary anteroposterior hypoplasia (54% of DS patients have Angle Class III tendencies);
- Maxillary transverse hypoplasia (65% of DS patients have posterior crossbites);
- Congenitally missing teeth (20 times more frequent in DS patients than in the general population);
- Tooth size discrepancy (high degree of frequency of interference with ideal interarch coordination);
- Open bite (interfering with proper mastication);
- Impacted teeth (10 times more canine impactions than the non-DS population);
- Transposed teeth (15% with Mx.C.P1 transpositions, compared to 0.3% in the general population);
- Tongue thrust and protrusive tongue posture (muscle hypotonicity and joint laxity are frequently present requiring speech and myofunctional therapy);
- Gingival excess and periodontal infection;
- Chewing difficulties leading to frequent choking episodes.
The above conditions benefit from timely orthodontic intervention; frequently, a two-phase or multiphase treatment program is beneficial to assist in early correction of maxillary transverse deficiency and Class III malocclusion. In addition, if a child has more than one of these frequently occurring conditions, advanced interdisciplinary therapy will be required with a well-coordinated and experienced dental team, including critical treatment planning input from the orthodontist.
Technologic advances in orthodontics have made it possible for orthodontists to create a treatment environment that welcomes children with special needs and treatment requirements. The following technologic improvements help all orthodontic patients, but some are specifically useful for patients with DS:
- Impressions using quick-set materials with fun flavors—these may reduce the tendency for activation of the more sensitive gag reflex frequently experienced with DS patients;
- Easy bonding of brackets rather than more complex and uncomfortable banding procedures;
- Self-etching primer, to reduce the taste of conventional etchants and glass ionomer cements that can be used in the oral environment in which it is difficult to maintain a dry field for several minutes at a time;
- High-memory wires, allowing a longer activation interval between appointments;
- Self-ligating brackets, which allow a more patient-friendly activation appointment;
- Advances in orthognathic surgical techniques that are less invasive and more predictable;
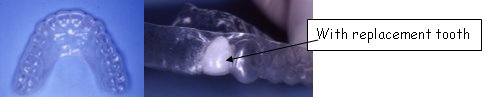
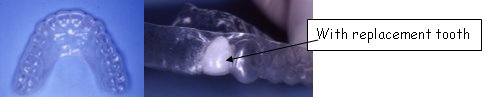
- Current reliability of implant replacement of congenitally absent teeth, which greatly aids the overall prognosis for patients with DS;
- Reversible implant anchorage devices to minimize compliance requirements needed for successful tooth movement.
Summary
The orthodontic specialist has many treatment management tools and skills to improve the quality of life for the patient born with DS. The use of the new Supplemental History form available through the American Association of Orthodontists (AAO) allows the parents to provide helpful descriptions of details about their child that will allow the dental team to create a health care environment that is more sensitive and comfortable for both the parent and the DS child.
With the technological advances available and the increasing numbers of kids with DS seeking orthodontic care, our orthodontic residency programs need to include training for orthodontic treatment of DS patients similar to the training available for cleft palate team participation. Currently, the AAO's Council on Education is assessing the role of residency programs training future orthodontists to handle the unique needs of patients with DS and patients with other special needs. Doctor and staff training with clinical updates would be made possible at university centers. Through more frequent journal articles and presentations on this subject, orthodontic specialists might become more comfortable setting aside the extra time needed to manage the requirements of children with DS.
The orthodontic specialty is rapidly becoming aware of the need for its leadership in developing an optimal interdisciplinary setting for providing patients with DS with the advanced dental care available and needed to improve the quality of their lives. With many excellent residency programs in North America, one could easily envision orthodontic specialists taking the lead in the development of interdisciplinary DS treatment teams. In turn, those teams could contribute to existing guidelines that would aid in future treatment approaches, which would be specifically designed for the multifaceted dental problems of the DS patient.2 Although the optimal treatment of DS patients presents complex challenges for orthodontic specialists and their teams, the fulfillment of applying the best available orthodontic skills to help children with DS is uniquely rewarding. Providing the care and enjoying the fulfillment are experiences in which all orthodontists and staff must be adequately trained.
References
- Pilcher ES. Dental care for the patient with Down Syndrome. Down Syndr Res Pract. 1998; 5:111-116.
- Desai SS. Down Syndrome. A review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84:279-285.
- Cohen I. Health care guidelines for individuals with Down Syndrome. Down Syndr Q. June 1996; 1:2.
Common Dental Conditions — January Meeting Recap. Reprinted from UPS for DownS Newsletter, February, 2006, p. 3, 5-6.
In January, Orthodontists Dr. David Musich (pronounced "music"), Dr. Matt Busch and orthodontic assistant, Sherri Schultz, gave UPS for DownS a very informative presentation entitled: Orthodontic Possibilities for Children with Down Syndrome.
Dr. Musich stated that nearly 100% of children with Down syndrome have major dental or orthodontic problems. Dr. Musich and his staff are committed to getting more taught in dental schools about treatment approaches for children with special needs.
Common Dental Conditions
The staff reviewed several common dental conditions and terminology associated with Down syndrome:
- Children with DS are ten times more likely to have congenitally missing teeth than children without DS. The most common teeth to be missing are third year molars, pre-molars and lateral incisors. Dr. Musich pointed out that teeth missing are a problem that needs to be addressed.
- Individuals with DS also have a higher incidence of impacted teeth. One in four children with DS has impacted eye teeth, the teeth on either side of the front two teeth.
- Thirty to fifty -five percent of patients have smaller or underdeveloped teeth, with short roots.
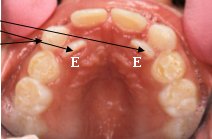
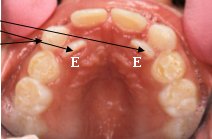
- Ectopic teeth are also common. It is often caused by retained baby teeth. For example, a retained baby molar is three times the size of the permanent tooth that should replace it. Ectopic teeth may erupt in the palate just behind the other teeth, or in the upper outside of the gums due to a narrow upper jaw or lack of arch in the perimeter of the mouth.
Dr. Musich explained that the term oversized tongue refers to the tongue's laxity due to hypotonia, or low tone that is common in individuals with Down syndrome. Because of this, the tongue has a tendency to push forward out of the mouth, making it appear oversized for the mouth. This can cause mouth breathing and dry mouth which contributes to dental problems, such as periodontal disease. Another common condition is a crossbite. This misalignment of bite can occur in the front or the back of the mouth. This is caused by an imbalance in the amount of jaw growth relative to the growth of the midface, in individuals with Down syndrome. Dr. Musich explained that in a proper bite, the upper jaw should sit on top of the lower jaw the way a lid fits over a jar. Because of the underdevelopment of the upper jaw both in width and length, sixty- five percent of individuals with DS have what is called a Class III underbite. In this condition, the lower jaw is longer than the upper jaw resulting in the upper front teeth falling behind the lower front teeth when the mouth is closed. If this appears at a young age, it should be brought to the attention of an orthodontist, as it is something that will need to be followed and worked with over time.
Treatment is Possible
Although there are many common dental conditions to be aware of in children with Down syndrome, Dr. Musich noted that 80% of patients with Ds in his office respond to orthodontic treatment alone, without need for more invasive surgical intervention. It is key to address the issues before growth slows down. Dr. Musich explained that the midface typically stops growing about 13 years of age. The lower jaw however continues to grow until growth is done, typically 16 -18 years in women and early 20's in men. The typical age to see an orthodontist is 8 years old. An initial visit can be done as early as 4 or 6 years of age. Even at 11, 12 or 13 however, there is still a tremendous amount of skeletal growth in a child to take advantage of orthodontic treatment.
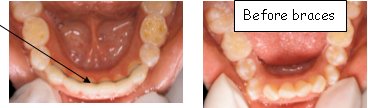
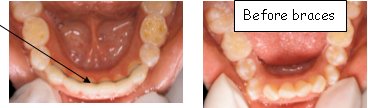
Commonly, patients are treated in phases aimed at expanding the upper jaw to make room for the teeth to align more normally.
Each patient should have care integrated with his/her dentist and the orthodontist. Because orthodontic treatment is gradual over a long period of time, usually 12 to 24 months, the orthodontist can start slow to be sure the patient is adjusting to the process. They can make up time as needed, as long as they are building on each step along the way. There can be long term consequences not treating an underbite. Parents need to watch their child's eating to note any problems. If they are having difficulties with chewing, or are choking on food, it is important to see an orthodontist. Learn what needs to be done and map out a treatment plan.
Establishing an Orthodontic Record
A number of different measurements are taken to establish the patient's skeletal pattern and baseline before any orthodontic treatment begins. These are referred to as records appointments. These appointments may be broken into a few visits.
Impressions of the patient's teeth are taken as study models. To help a child become comfortable with making an impression in the mold material, Dr. Musich's office will often first make an impression of the child's hand so that they can get used to the impression medium. The child can then see the resulting hand impression at the next appointment. On occasion, the trays are sent home with the child so that they can practice how it feels using yogurt in the tray as a stand-in for the medium.
Full mouth, panoramic x-rays are also taken. These show whether teeth are impacted or missing. Side view x-rays for lateral cephalometric analysis allow the orthodontist to measure landmarks in the child's jaw growth, to note over or under development of the jaw. A posterior-anterior head x-ray (front-back) shows whether the patient needs upper jaw expansion and how much is needed to correct a mismatched bite. A wrist plate x-ray is taken to see how much growth the patient has left to maturity to determine treatment options. And photos of the patient's teeth are taken to note spacing and wear marks.
A First Impression is a Lasting Impression
This group of orthodontists believes that teamwork is important in working with children with special needs. Dr. Musich, Dr. Busch and staff work with each family to create a comfortable atmosphere for each child. In order to make each patient as comfortable as possible with the process and treatments, they begin with supplemental questionnaire for parents developed by one of their orthodontic assistants, Jolette Porter. The form asks parents about their child's condition and how it affect's their behavior, it asks about the child's fears, dislikes, prior experiences and strategies that help the child open up to new experiences. A welcome letter and health history questionnaire are sent home before the first appointment so that parents are not rushed when completing them and can have time to think about the questions asked. They then review the form with the doctor at the initial visit.
Dr. Busch shared a variety of ways they work together with the family to assure the child's comfort. Some of those include: sunglasses to shade patients from the overhead lights, role playing the visit at home to practice what it would be like, and 'show and tell' with other patients who are willing to help the new ones along. Experienced patients are often very receptive to having new patients watch and learn about the treatment experience.
Some patients need to know exactly what will happen next, and others do not want to know. They try to accommodate each patient's comfort level. Some patients may need surgical intervention, especially if older and growth has stopped. Some may be very fearful of any kind of dental treatment, making it difficult to undergo months of orthodontic treatment. Every patient must weigh the cost-benefit to treatment in their unique scenario, when determining their possibilities.
Dr. Musich suggested that parents ask any orthodontist they are considering whether it is in their comfort zone to treat patients with Down syndrome. Dr. Musich asked several orthodontists and dentists whether they treat patients with special needs. He compiled these into a list which he included in his handouts.
Common Treatments
The midline of the roof of the mouth represents a suture that keeps moving as a child is growing. Until that growth stops it is possible to exert pressure with an expander to widen the palate to allow for better teeth alignment.
Many parents in the audience attested to the ease with which their children became used to this treatment approach. This is done with the most common treatment appliance, a palate expander, which is a metal device that fits across the palate, and is expanded in small increments with the turn of a key. Parents are taught when and how much to turn the key to change the pressure. Partial braces are available today in many colors which children love. A removable traction appliance, which applies elastic traction, can be used to accelerate forward growth of the upper jaw. There are also removable and fixed retainers which may also hold replacement teeth.
Is this for us? Points to Remember
- Monitor your child for difficulties with chewing, or choking. See an orthodontist if these are occurring frequently.
- Visit an orthodontist sooner rather than later to learn what problems may exist, and the options available to remedy them. An early visit allows time for your child, and you, to become comfortable with the prospect of treatment.
- Timing is important. If possible, address issues before growth slows down.
- Discuss treatment options fully with your child's orthodontic specialists to weigh the cost and benefit to treatment in your child's unique situation.
- Be sure that your child's dentist and orthodontist are providing your child integrated care.
- Provide your orthodontic team with information about your child's fears and anxieties, strategies that have worked and those that have not, and any other information that would better help the dental team treat your child.
- Work with your orthodontist office to help put your child at ease.
- SMILE! There is nothing better to help someone feel good.
David R. Musich, D.D.S., M.S.
Matthew J. Busch, D.D.S.
1701 E. Woodfield Road, Suite 500
Schaumburg, IL 60173
(847) 517-1333
Orthodontic possibilities for children with Down Syndrome. Drs. Musich, and Busch & orthodontic assistants Jolette Porter and Sherri Schultz. Presented to Ups for Downs Parent Group, January 24, 2006.
- Common dental conditions and terminology associated with Down syndrome:
- Missing teeth
- Impacted teeth
- Short roots

- Ectopic teeth (transposed position with another tooth)
- Retained baby teeth
- Crossbite (Anterior/underbite and posterior)

- Oversized tongue
- Jaw growth imbalance. Class III with underbite

- Helping to make the dental (ortho) office feel comfortable and safe (supplemental questionnaire)
Patient's Name:
Date:
On your health history you have identified your child with:
Would you please help us understand more about this condition and how it might affect your child in a dental/orthodontic setting?
- Could you tell us about the condition your child has and how it affects his/her behavior.
- Please describe any significant fears or anxieties that your child may experience during visits to health care professionals (including dental).
- Has the anxiety or fear prevented any necessary treatment? Please describe.
- Are there any strategies that help your child open up to new experiences such as a visit to a new doctor (Examples: show and tell, humor, going very slowly; modeling with parent or other sibling, other examples)?
- Are there physical disabilities that need to be taken into consideration? (Examples: Difficulty with fine motor skills)
- Are there learning disabilities that need to be taken into consideration? (Examples: Auditory processing difficulties, sensory integration dysfunction, or speech and language difficulties)
- Any additional information that might help us to provide a positive office experience for your child?
- Orthodontic study records:
- Study models

- Panoramic x-ray

- Lateral Cephalometric analysis

- Postero-anterior head x-ray

- Photographs

- Wrist x-rays to assess physical maturity

- Orthodontic Appliances useful to treat dental conditions of kids with Down syndrome.
- Expanders to widen palate

- Partial Braces to align incisors

- Removable traction appliance to provide elastic traction to accelerate forward growth of upper jaw

- Removable retainers
- Fixed retainers
- Frequently asked questions by parents and kids:

- Will braces or the expander hurt?
- What do you mean by orthodontic records?
- How do the orthodontic appliances affect speech?
- My child has a lot of anxiety-what can be done?
- What will my child be able to eat with braces on?
- Will my child have more cavities while in braces?
- Most of my child's teeth are baby teeth-aren't they too young for braces?
- Has any new technology helped to reduce the "hassle factor" related to braces?
- Your specific questions:
Thank you for your interest.
More Smile for Patients with Disabilities Orthodontists open doors to accommodate patients with special needs.
From the Bulletin of the American Association of Orthodontics, Jan/Feb, 2004
"I do believe that Angie taught everyone on the team a few very important things along the road. A person with a disability is still just a person who deserves to be treated with dignity and respect. Never assume someone doesn't understand what you're saying because they don't speak as well as you. If you have the patience to really listen to what they have to say, you will realize that they have likes and dislikes, friends and interests, hopes and dreams just like the rest of us. If you give them a chance, you will be amazed at some of the gifts they have to share and how they can bring you so much joy."
Angela's mom, Mrs. Picchi
Web Wanderings
Prenatal Test Puts Down Syndrome in Hard Focus by Amy Harmon. May 9, 2007. URL: http://www.nytimes.com/2007/05/09/us/09down.html?ex=1336363200&en=ccf8eef18ff478e4&ei=5088
DETROIT — Sarah Itoh, a self-described "almost-eleven-and-a-half," betrayed no trace of nervousness as she told a roomful of genetic counselors and obstetricians about herself one recent afternoon.
She likes to read, she said. Math used to be hard, but it is getting easier. She plays clarinet in her school band. She is a junior girl scout and an aunt, and she likes to organize, so her room is very clean. Last year, she won three medals in the Special Olympics.
"I am so lucky I get to do so many things," she concluded. "I just want you to know, even though I have Down syndrome, it is O.K."
Father's Journal
My wife's fault
Emmanuel leads the rosary and is learning to serve Mass. He goes to confession every time his mother goes, which is all the time.
|
|
[...] About 90 percent of pregnant women who are given a Down syndrome diagnosis have chosen to have an abortion.
[...] There are many couples who do not want to have a baby with Down syndrome," said Deborah A. Driscoll, chief of the obstetrics department at the University of Pennsylvania and a lead author of the new recommendation from the obstetricians' group. "They don't have the resources, don't have the emotional stamina, don't have the family support. We are recommending this testing be offered so that parents have a choice."